Huntington's disease is caused by a polyglutamine repeat which is a type 1 trinucleotide repeat disorder. A polyglutamine repeat is the adding of the CAG triplet codon which codes for the amino acid glutamate when the cell divides. The Huntingtin protein is present on the gene locus 4p16.3 and under normal conditions does still contain CAG repeats, the normal non-pathological range of repeats is 6-34 repeats of CAG. It becomes pathological at 36-121 repeats. It is inherited but also progressive so the number of repeats the previous generation has could actually increase with the next generation. It is therefore possible for the previous generation to be in normal range with 34 repeats but the next generation could have 36 repeats and develop Huntington's disease.
Lets break these ranges down a little more because there are a lot of gaps between ranges. Up to 26 repeats never causes HD, people with over 40 repeats will develop HD later in life. Those with 36-39 repeats may or may not develop HD, it is impossible to tell if or when they will get symptoms. These leaves a sizeable gap at 27-35 repeats which is the intermediate range. This range is where the person within this range does not get the disease but their offspring could have an expanded CAG repeat to a range that could or will lead to HD.
There are little to no symptoms until midlife often, onset is usually between 30 and 50 and if the repeat is high, into the hundreds, juvenile onset occurs and it is very severe. Death is usually 10 to 20 years but around 5 years if it is juvenile. Death is often due to respiratory failure but high instances of suicide are seen as well as infection at least in part due to the difficulty in being hygienic.
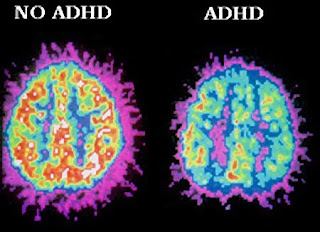
The huntingtin protein is a cytoplasmic protein and has its function in the brain, mostly in the cortex and striatum so these areas become most affected by the polyglutamine repeat in the huntingtin protein. This leads to a specific set of symptoms, in 90% of cases a chorea occurs, chorea is characterised by jerky involuntary movements especially in the face. Bradykinesia is a lack of movement and dysphagia is trouble swallowing. However, the main symptom is other movement symptoms that progress to an ataxia. Ataxia is a complete loss of control of most bodily movements. Loss of short term memory and a level of psychosis. There are also significant changes in personality, people can quickly change to become agitated and irritable and aggressive. Depression, mania and complete social withdrawal can also occur.

Not only is this disease inherited but it is also autosomal dominant which means only one parent needs to have or carry the disease for the offspring to also develop it. The the striatum inclusions of plagues in the cytoplasm and nucleus of neurons is rare but in HD the huntingin protein mutates at the N terminus which then aggregate in the nucleus and cytoplasm of neurons as well as in the dendritic spines. Noticeable changes to the dendritic spines appear in HD, at mid stage the GABA/enkephalin medium spiny neurons are first affected but many spiny neurons have abnormal bends in the distal dendrites and increases in branching of the dendrites. The spines coming from these dendrites increase in number and increase in size. The spines are the parts on the dendritic branches that form synapses with the presynaptic neurons. This increase could explain the involuntary, uncoordinated movements, because an action potential from presynaptic neurons activate more spines causing more frequent action potentials. In late stage HD the dendrites become truncated, leaving some pre-synaptic terminals behind and the spines decrease in density so there are less synapses along the truncated dendrite. Despite this there is still an increase in number, which suggests that degeneration of neurons in the striatum leads to a compensatory response of the neurons that are left to increase spine density and dendritic branch density.


If you remember back to the pathways post, the changes in GABA transmission make sense. The striatum releases GABA to inhibit the external globus pallidus but this does not occur in HD so the external globus pallidus uses GABA to inhibit the sub-thalamic nucleus so it cannot use glutamate to activate neurons in the internal globus pallidus which would usually be inhibiting the thalamus vi GABA to prevent the thalamus signalling to the cortex to cause movement, this is the indirect pathway so inhibiting it leads to unwanted, involuntary movements. In addition to this, there is an area of the striatum that signals to the substantia nigra pars compacta using GABA and enkephalin to reduce the amount of dopamine released to the striatum. If this GABA release declines excess dopamine will be released to the striatum, in the direct pathway this means that GABA is released to the internal globus pallidus inhibiting its neurons from releasing GABA to the thalamus thus allowing the thalamus to signal to the cortex to allow movement, but because it is excess dopamine it would lead to excess and most likely uncoordinated movements because the frequency of signal would be much higher leading to chaos where timing of a movement appear.

Having said all this, the neurons that contain enkephalin and GABA and project to the external globus pallidus (indirect pathway) are more vulnerable than the medium spiny neurons that contain substance P and GABA and project to the internal globus pallidus. This suggests that the indirect pathway dysfunction increasing involuntary movement is more involved than the direct pathway. Another interesting point is that the huntingtin protein is expressed ubiquitously throughout the body and brain yet the damage lies very selectively in the striatum. It is more selective than that because interneurons seem to be largely unaffected and why do GABA/enkephalin medium spiny neurons become altered first?
Huntingtin protein:
I have mentioned this and we are basically saying that this protein is causing this debilitating disease by mutating, then I have talked about the affects this mutation has on the neurons leading to neuropathology, but what I have not done is talked about the pathology of the protein. That is because the function of huntingtin has not been assigned (we do not know) and the pathogenesis is poorly understood. The protein has phosphorylation sites near the N terminus that regulate clearance of the protein and a sequence for ubiquitin binding to degrade huntingtin and a site for sumoylation which regulates the proteins stability and activity. There is a sequence next to this which allows the protein to associate with mitochondria, golgi and ER. There is also a site for regulating the trafficking of vesicles and phosphorylation sites for cleavage of the protein, aggregation and vesicular transport. As it is also a nuclear and cytoplasmic protein it also contains a nuclear export signal to allow it to enter the cytoplasm. So do these things translate to clues about function? The regulator of vesicle trafficking and the protein having an association with HYP-C suggest it has involvement in intracellular trafficking and retrograde axonal transport (transport of things along the cytoskeleton back to the nucleus). It has association with proteins involved in vesicle endocytosis and membrane recycling plus it is present in synaptic vesicles, so probably has involvement in these two processes. Finally, it has been shown to inhibit acetyltransferase activity which decreases the level of histone acetylation at H3 and H4 when it its aggregated form. Acetylating histones loosens their coil on DNA allowing for faster transcription, so huntingtin could be involved in reducing the rate of transcription (histone deacetylase inhibitors reverse their deacetylation of histones).

Evidence suggests that mutated huntingtin proteins aggregate and then become involved in disrupting transcription. It was first shown that mutated huntingtin directly uncoupled the Sp1 promoter from its TAF4 coactivator by binding to TAF4 thus stopping transcription that is initiated by Sp1 promoters. After this it was shown that TAF4 is present in TFIID which interacts with CREB. Interfering with CREB interactions would reduce the transcription of a wide range of protein mRNA in neurons, therefore interfering with CREB will usually cause neurodegeneration. It has been shown that PGC-1alpha is heavily downregulated by mutant huntingtin in early HD and it also has a CRE site for CREB. PGC-1alpha is a transcriptional coactivator that regulates oxidative phosphorylation in mitochondria. Therefore, interfering with the transcription of this coactivator leads to mitochondrial dysfunction. Striatal neurons seem to be very vulnerable to mitochondria dysfunction because decreased striatal metabolism is seen years before HD symptoms appear. PGC-1alpha inhibition limits striatal neurons ability to respond to the metabolic demands needed to keep responding to movement signals, they may be more vulnerable because constantly inhibiting unwanted movement requires lots of ATP through oxidative phosphorylation in the mitochondria. The lack of ATP available causes neurons to lose their function in the brain and cellular functions are lost that require ATP eventually leading to neuron death (neurodegeneration). In addition to this there are direct toxicities from mutant huntingtin, it targets processes such as axonal transport which require high ATP levels and mutant huntingtin with a higher number of repeats also changes the depolarisation of mitochondrial membranes. Further evidence is shown in postmortem studies of HD patients as the expression of PGC-1alpha in stiatum is 30% lower than normal but no significant change was found in the level in the hippocampus or cerebellum.
Some good news from this is that lentiviral injections of PGC-1alpha into the striatum of transgenic mice and found that neuronal volume was 27.8% higher in the striatum of those injected over those not injected. Suggesting some neuroprotective effect of PGC-1alpha and use as a potential treatment.
Whether mutated huntingtin is a true histone deacetylase remains to be answered but treatment of HD with HDAC inhibitors in mice is showing a countering affect to mutant huntingtin and it certainly has some sort of involvement in inhibiting transcription. The drug Selisistat has found to be safe and tolerable in phase II trials but as far as I can tell is still in phase III, I will update this if I find any information.
Current treatment:
There is no cure as of yet and neurodegenerative disorders seem nearly impossible to cure so far but it is always just a matter of time. The main treatments are for the psychiatric symptoms and tetrabenazine is used for the chorea to control the involuntary movements. it is unknown how tetrabenazine reduces chorea but it is believed to be because it is a reversible inhibitor of vesicular monoamine transporter 2 (VMAT2) which means monoamines, importantly dopamine, but also noradrenalin, histamine and serotonin cannot be loaded into synaptic vesicles so there is a lower release of monoamine to the post synaptic membrane meaning fewer action potentials. This is a pretty good hypothesis to me, it just has not been proven.
Antidepressants are used for depression and haloperidol has been used for the psychosis and hallucinations, however chlorpromazine or sulpiride are more used now. These may have some effect on the movement disorders because they antagonise the D2 receptor so have a duel effect, this is why they are more used than the better drug clozapine because it is a D4 antagonist so only treats the psychosis. Lithium ca be used to prevent the mania/mood swings and benzodiazepines will help with any anxiety and excess movement because they are sedatives.
Future therapy:
I am going to mention an important future therapy target for HD but the diagram shows a few more that are also viable.
Neurotrophic factors- The first is brain derived neurotrophic factor (BDNF), in HD context BDNF usually get released to the striatum by cortical neurons to aid in neuronal survival in the striatum. BDNF is also released in the nigrostriatal pathway and in HD the levels of BDNF are reduced compared to normal, probably due to reduced transcription (CREB is needed at promoter site 4). It is shown that the protein HAP1 interacts with BDNF but the level of interactions is reduced in the presence of mutated huntingtin. Huntingtin has been shown to facilitate BDNF transport and mutant huntingtin stops this facilitation. Additionally, BDNF elicits its effects through tyrosine related kinase B receptor (TrkBR) to have effects of transcription. In HD the number of TrkB receptors are downregulated, it is unclear how mutant huntingtin downregulates TrkB but the TrkB gene is under CREB regulation. It seems to be a future therapy with studies using adenoassociated viral injection to locally increase BDNF levels in the striatum and it has shown to be neuroprotective and and aid motor function, but this has been known over 10 years. Annoyingly, in 2014 new evidence came to light that showed no decrease in the level of BDNF produced in the cortex and the level received by the striatum is normal and the abundance of TrkB is normal. However, the same study also shows that the TrkB signalling was impaired rather than it being downregulated. Whay was signalling impaired?
Well BDNF also acts on a receptor known as p75NTR which directly acts on GDP dissociation inhibitor which inhibits the action of GTPase (RhoA). RhoA also activates associated kinases to phosphorylate PTEN which is a phosphetase that dephosphorylates the ring of phosphoinositide (PIP3) to stop its signalling cascade. PIP3 is part of the TrkB signalling so its inhibition could explain the TrkB signalling impairment in HD. Inhibition of the p75NTR receptor, The RhoA associated kinase and PTEN separately all restored TrkB function and synaptic plasticity in HD mice. There was no upregulation of p75NTR so the effects must be due to increased BDNF binding to the receptor or upregulation somewhere else. As it turns out, PTEN expression is much higher in HD mice, it is unclear why but it may be due to mutant huntingtin altering the proteins trafficking causing higher concentrations. The therapy is moving towards inhibiting PTEN and/or p75NTR.