Stimulants
as an ADHD treatment
Methylphenidate is a potent stimulant, known by the brand name Ritalin©, it is effective in 80% of ADHD patients and shown to noticeably improve symptoms. It is a noradrenalin-dopamine reuptake inhibitor that acts most potently on dopamine reuptake membrane transporters to block them. Methylphenidate has a pharmacophore (figure 2A) that binds to DATs at one site and binds in three ways (Volz, 2008). The nitrogen from the amine forms a hydrogen bond, the ester bond forms one or two hydrogen bonds with arginine on DAT and the phenyl ring forms a hydrophobic interaction by slotting into a hydrophobic binding pocket on DAT (Volz, 2008). Figure 2B shows dopamine entering between transmembrane domains 4 and 5 of the DAT1 transporter, this causes a conformational change which releases dopamine into the cell, binding of methylphenidate changes the confirmation of the transporter such that dopamine can no longer pass through the transporter. This prevents the reuptake of dopamine back into the presynaptic neuron, this means the concentration stays high enough to act on post synaptic receptors for a prolonged period of time.
Dopamine is a modulatory neurotransmitter involved primarily in inhibition so methylphenidate restoring adequate dopamine to the mesocortex returns the ability to attend to stimuli. It also causes increased inhibition in the prefrontal cortex, this improves the persons ability to filter out any distractions and inhibit inappropriate behaviours and therefore enhances cognition to within normal range (HuntMD, 2006). Motor problems such as fidgeting are also inhibited through increased dopamine in the nigrostriatal pathway.
Other stimulants include Dexamphetamine and Lisdexamfetamine, these are amphetamine stimulants that are used in ADHD when methylphenidate has been contraindicated. Lisdexamfetamine is the inactive prodrug administration of dexamphetamine. They act by reversing all monoamine reuptake transporters compared to methylphenidate which is selective for noradrenalin and dopamine (Wallace, 2012). These drugs also increase the release of monoamines by increasing the activity of vesicular monoamine transporter 2 (VMAT2) which is an antiporter, moving monoamines into vesicles in exchange for protons, as well as inhibiting monoamine oxidase to prolong the action of monoamines (Wallace, 2012). These amphetamines improve function in the right caudate nucleus and prefrontal cortex, benefiting both motor and cognitive deficits (Spencer et al., 2013). They show clinical efficacy in a similar number of cases to methylphenidate (Parker et al., 2013), However, are used less frequently due to worse adverse effects, including mood swings, aggression and hyper-excitability (Punja et al., 2012).
Atypical
antidepressants as an ADHD treatment
Mirtazapine is an atypical antidepressant with a tetracyclic structure
and the overall function of increasing the action of
serotonin/5-hydroxytyptamine (5-HT) and noradrenalin. It affects ADHD by acting
against the mutations in 5-HT transporter and the HTR1B receptor mentioned
above. Mirtazapine works by blocking 5-HT2 and 3 receptor subtypes, these are
post synaptic G protein coupled receptors (GPCRs) and ion channels
respectively. Whilst simultaneously increasing 5-HT1 receptor activity. These are
pre and post synaptic GPCRs that decrease cellular responses through inhibiting the cyclic adenosine
monophosphate second messenger pathways via phosphodiesterase (Anttila and Leinonen, 2001). It has been suggested that increasing the
serotonin to bind to 5HT1 receptors decreases cellular response further, thus
reversing the emotional dysregulation in ADHD patients, such as aggression and
being antisocial (Davis and Wilde, 1996). Mirtazapine has been shown to be <40%
effective in the most effected age groups and 50% effective in adults (figure
3A). 5-HT1B and 5-HT2B receptor types have very similar structures, so
mirtazapine blocking one and activating the other is intricate. Figure 3B shows
that the binding pocket of 5-HT2B is smaller than in 5-HT1B so mirtazapine
blocks the pocket, whereas in 5-HT1B mirtazapine binds in the pocket to
modulate the receptor, still leaving space for the binding of serotonin (Davis and Wilde, 1996).
In a healthy person there is no beneficial emotional regulation and it
does not increase mood, so it only works in someone who has depression or ADHD (Schüle et al., 2002). However, whether administering to a healthy
person or ADHD patient, it elicits the same adverse effects. One of the most
significant adverse effects is serotonin syndrome, this is an excessive
increase in serotonin leading to tremors, severe hypotension and hyperthermia
which can be fatal (Boyer and Shannon, 2005). Other adverse effects include tachycardia,
headaches and extreme drowsiness.
Summary
ADHD has very significant cognitive and emotional impairment, which leads to the loss of attention and excessive motor action such as being easily distracted and fidgeting respectively. These symptoms are associated with the pathological features of a smaller brain size, significantly fewer fibres in the corpus callosum and changes in the right caudate nucleus as shown by Castellanos’s team and the Catherine studies. The treatments for ADHD focus on reversing the symptoms and not on the pathological features because little can be done about these. Methylphenidate is a dopamine, noradrenaline reuptake inhibitor that acts primarily on the DAT1 dopamine transporter to prevent dopamine re-entering the presynaptic membrane to prolong the activity of dopamine. This leads to cognitive enhancements to normal functioning. Mirtazapine increases the action of serotonin on 5-HT1, blocking 5-HT2A and 5-HT2B at the same time. The adverse effects are significant for a child, however, the benefits the drugs have on the cognitive and emotional symptoms exceed the adverse effects.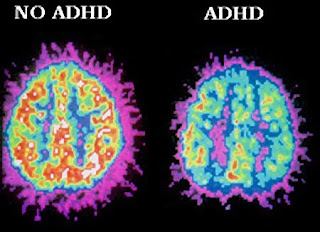





No comments:
Post a Comment